Over the past few months KevinMD has posted a series of articles by me on what I call the “Crisis in Primary Care.” (BTW, I was not a PCP.) Most recently have been a few posts related to direct primary care. They have generated many comments – some pro and some con. I have greatly appreciated everyone’s interest; it makes it worth the time to write. So thanks.
My fundamental belief, contrary to some comments, is that PCPs are much more than providers of “simple” stuff. They are more correctly specialists that deal with the very complex. Comprehensive primary care includes wellness and health maintenance, prevention and risk management strategies, attending to the episodic events that occur in life, and the care of those with complex chronic illnesses including coordination of care when a specialist is needed. It also includes developing a strong relationship between doctor and patient, building trust along the way and offering true healing. This means that the PCP can competently handle the vast majority of our health needs.
But all of this takes time and when the current practice business model forces the PCP to see 25 or more patients per day, there is just not enough time. Direct primary care (DPC) is one way to regain that time. It is not the only way. I plan to discuss some other approaches in later posts.
A few themes have arisen repeatedly in comments from these posts about direct primary care. One is that there is a difference among the terms DPC, membership, retainer, and concierge. But to me, they all mean essentially the same thing – fewer patients per doctor and therefore more time for the patient with the doctor which equates to better care. There does seem to be a degree of concurrence that DPC and membership are terms most often used for those practices that cost less per month or year and retainer and concierge for those that cost more. (There are a very few that charge a huge fee; I discount these as giving the term “concierge” a negative connotation to many.)
Among the most common other themes from the perspective of a patient are: DPC is too expensive, especially for those of lesser means. DPC is an added expense if you already have primary care coverage by your insurance (e.g., Medicare or company policy). The PCP “abandons” patients when converting to DPC and does it because he or she is greedy. And the question – Is the care quality really better and are costs really lowered? Some thoughts on each.
First, DPC is certainly not for everyone – patient or doctor. But it is one model and it has proven very effective for some.
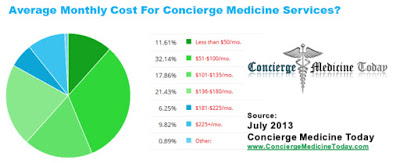
Expensive? It’s relative. The average American family spends $2237 per year for cable TV, internet and phone. A Starbucks a day adds up. A parking space per month in a downtown lot is probably more than the DPC doctor. It is about prioritizing our personal expenditures. I also postedan article using as examples three practices that have been termed “blue collar” in the popular press because the costs per month are relatively low, the service is high and with the added benefit of generic drugs at wholesale prices many patients can save handsomely. Two of them have noted that they have many uninsured patients. These practices are cheaper than urgent care clinics and much cheaper than the ER. One person commented that I cherry picked cheap Midwest practices; DPC in urban areas cost much more. That is likely true if only because rent and staff cost more. Here is a chart from Concierge Medicine Today related to costs across the USA.
Why sign up if you already have insurance that covers primary care? The question to answer for each person is whether it is worth the extra money to get more time with your PCP? A lot more time. My PCP converted about five years ago. I was ticked off that I had to pay an extra $1500 a year since I am on Medicare and primary care is mostly covered. Some of my friends decided to not convert with him. Others decided as I did to pay up. My wife’s PCP converted to a retainer approach a few years ago. Same thoughts. But it has been worth the price – to us. But probably not for everybody. Again, it is a question of your priorities.
What about abandonment? It is another of those questions where the answer depends on your perspective. A group practice I know planned to convert and announced it to their patients. Soon articles appeared in the local paper about “greedy” doctors and patients who would be left without a doctor. But everyone who wanted to find a new PCP did so quickly – often with help of their former PCP who guided them to an appropriate doctor. Of course, in say a rural community where there is just one provider, it would be a different story. An analogy given me by Dr Josh Umbehr might be useful. Consider a 60 watt bulb. Try to push more voltage through it and it will burn out and there is no longer any light at all. Run it as it is supposed to be and it will last a long time. If the doctor is burned out and gets sick or just quits, that is not abandonment. It is actually worse.
And the greedy doctor issue? When a PCP with a busy practice converts, they often end up with a much lower income, at least at first. Read some of Dr Rob Lamperts postsabout what happened to his income including a one about his application for health insurance and for Medicaid. Later their income may rise and sometimes it will be more than before. From that same Concierge Medicine Today article – 73% of concierge or DPC physicians earn less than $200,000 per year. But it is really not about more money; it is about more time for each patient.
Quality up and total costs down? I wrote about this in my last post; here is a summary. It is hard to find other than anecdotal data with individual practices or even group practices. MDVIP [which is not a DPC practice since it still takes insurance in addition to a retainer] is a practice model that lowers the number of patients to doctor to about 500:1. Among the about 700 affiliated doctors there are about 215,000 patient members, enough to do some observational studies. They have found that quality measureslike blood pressure control, diabetes control, immunization percentage, screening for cancer, etc. are substantially better than a comparable group of individuals not in their network. Similarly, there is a very substantial reduction in total medical care costs of $2551 per capita as a result of fewer referrals to specialists, fewer prescriptions, fewer hospitalization and fewer trips to the ER. As to satisfaction, perhaps the most important marker is that few individuals leave the practice.
Similarly, Iora Health, Qliance and AbsoluteCARE, organizations that like DPC practices lower the number of patients per provider, can demonstrate better outcomes with lower total costs. Here again the cost reduction is from fewer specialist visits, fewer hospitalizations and fewer ER visits among other parameters. Qliance, for example, has noted 35% fewer hospitalizations, 65% fewer emergency department visits, 66% fewer specialist visits, and 82% fewer surgeries than similar populations. (And before you tell me, I know that this reduction in costs may not directly accrue to the patient although it couldconvert into a substantial dollar savings for those with a high deductible policy. My point however is that fewer patients means better care which in turn means lower total costs.)
What about doctors? Is DPC for every PCP? I doubt it. When a practice is converted a lot fewer patients convert with it than might be expected – maybe 15-20%. Income will probably go down, at least initially. Some patients will feel the doctor is being greedy as noted above. There can be legal issues; the insurance commissioner may say it is essentially an insurance policy for primary care; a doctor is not an insurance company. Some sound advice would be important before embarking. Doctors are a cautious bunch; this is a big change. My bet is that, until patients actually start demanding more time and agreeing that this is a sensible approach, the total numbers of PCPs who convert will be modest.
Next time will be a different topic; what employers are doing to assure better care yet lower company costs. In many cases it too amounts to getting the PCP more time.